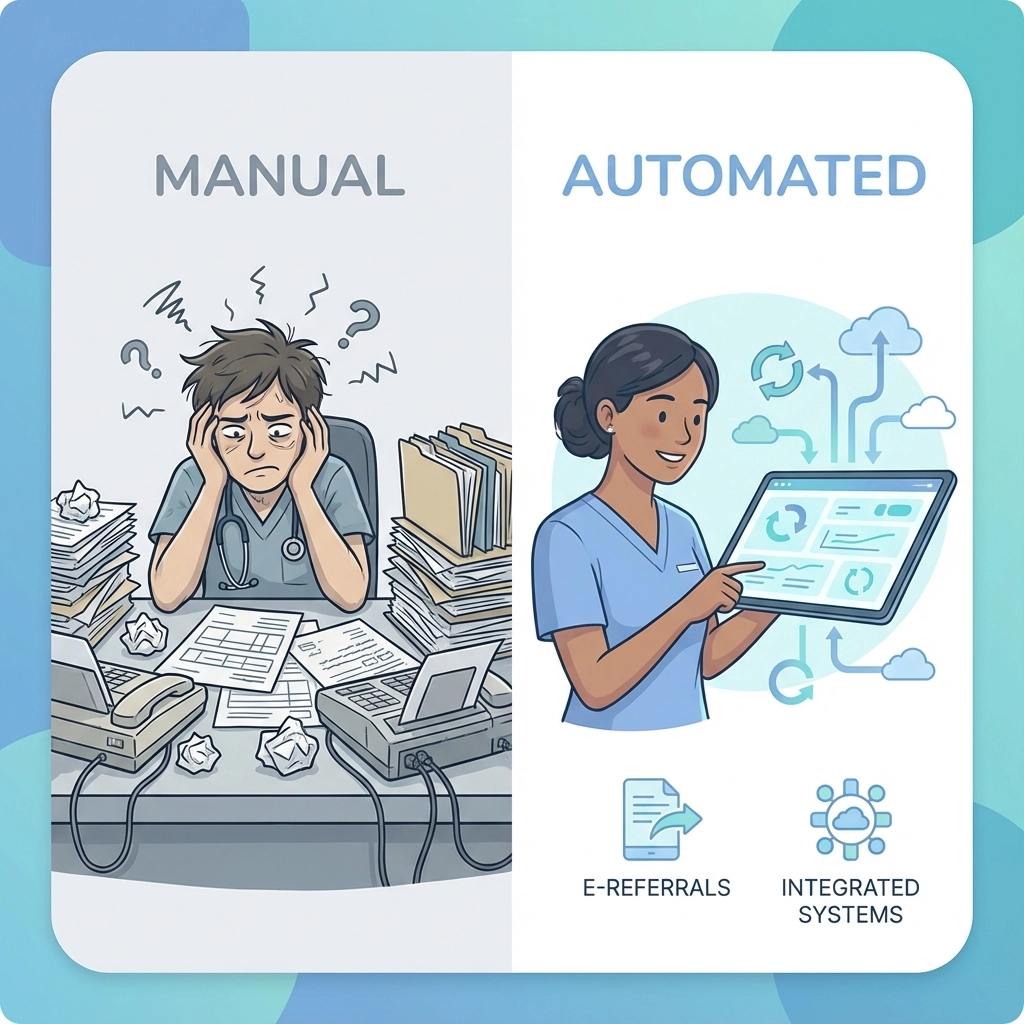
Implementing AI referral management in your skilled nursing facility doesn’t have to be overwhelming. With the right roadmap, you can transform your admissions process from a manual, time-consuming operation into a streamlined, automated system that fills beds faster and reduces administrative burden.
This comprehensive checklist breaks down the implementation process into manageable phases, ensuring your facility successfully adopts AI referral management technology while maintaining quality patient care.
Phase 1: Pre-Implementation Assessment (Weeks 1-2)
Stakeholder Engagement and Buy-In
√ Identify Key Stakeholders
- Admissions coordinators and directors
- IT department representatives
- Clinical staff who review referrals
- Executive leadership team
- Finance department for budget approval
√ Assess Current Referral Volume and Sources
Document your existing referral patterns, including which hospitals refer most frequently, average processing times, and current acceptance rates. This baseline data will help measure ROI post-implementation.
√ Evaluate Hospital Readiness
Contact your top referring hospitals to assess their digital referral capabilities. Many hospitals are already using platforms that can integrate with AI referral management systems, making the transition smoother.

Infrastructure and Compliance Audit
√ Review Current Technology Stack
- Document existing EHR systems and versions
- Assess internet bandwidth and connectivity reliability
- Inventory current hardware that staff will use to access the new system
- Identify integration requirements with existing software
√ Conduct Compliance Assessment
Ensure your facility meets all regulatory requirements for digital health data exchange, including HIPAA compliance, state licensing requirements, and any specific post-acute care regulations in your region.
√ Establish Implementation Budget
Factor in software licensing, training costs, potential hardware upgrades, and staff time for training and transition periods.
Phase 2: System Selection and Setup (Weeks 3-4)
Platform Evaluation Criteria
√ Core Functionality Requirements
- Real-time referral processing capabilities
- Integration with major hospital EHR systems (Epic, Cerner, Meditech)
- Automated insurance verification features
- Clinical assessment automation tools
- Bed availability tracking
- Reporting and analytics dashboards
√ Security and Compliance Features
Verify the platform includes HIPAA compliance, SOC 2 Type II certification, and encrypted data transmission. The system should maintain comprehensive audit logs for regulatory compliance.
√ Integration Capabilities
Confirm the platform supports FHIR and HL7 standards for seamless data exchange with hospital systems and your existing facility management software.
Data Preparation and Setup
√ Organize Facility Information
- Update provider directories with current specialty areas and capabilities
- Ensure bed availability information is accurate and up-to-date
- Prepare clinical protocols and admission criteria for system configuration
- Compile insurance acceptance information and verification requirements
√ Configure User Roles and Permissions
Set up different access levels for admissions coordinators, supervisors, clinical staff, and administrators based on their responsibilities in the referral process.
Phase 3: Pilot Program Implementation (Weeks 5-8)
Limited Rollout Strategy
√ Select Pilot Department
Choose a single high-volume department, such as orthopedics or cardiology, to test the system in a controlled environment. This allows your team to identify and resolve issues before full deployment.
√ Establish Success Metrics
- Referral processing time reduction
- Acceptance rate improvements
- Staff satisfaction scores
- Administrative time savings
- Documentation accuracy improvements
Core System Testing
√ Test Smart Matching Functionality
Verify the AI engine correctly evaluates patient needs against your facility’s capacity and specialization areas. The system should accurately match complex clinical requirements with available resources.
√ Validate Data Integration
Test automated documentation pull from hospital EHRs to ensure referral packets are complete and accurate. Verify that patient summaries, medication lists, and insurance information transfer correctly.
√ Confirm Communication Features
Test real-time messaging between your facility and referring hospitals. Ensure notifications, status updates, and escalation procedures work as designed.
Training and Change Management
√ Conduct Role-Specific Training Sessions
- Admissions coordinators: Focus on referral review and response workflows
- Clinical staff: Emphasize clinical assessment tools and documentation features
- Supervisors: Cover reporting, analytics, and oversight functions
- IT staff: Include troubleshooting and basic system administration
√ Create Training Materials
Develop quick-reference guides, video tutorials, and FAQ documents specific to your facility’s workflows and the chosen platform.
√ Establish Feedback Mechanisms
Set up regular check-ins with pilot program participants to gather feedback and identify areas for improvement before full rollout.
Phase 4: Full Implementation (Weeks 9-12)
Operational Workflow Integration
√ Implement Automated Processes
- Configure automated alerts for new referrals
- Set up escalation procedures for time-sensitive cases
- Establish protocols for handling system exceptions or downtime
- Enable automated insurance verification workflows
√ Establish Quality Assurance Protocols
Create procedures for regular data integrity checks, ensuring referral information remains accurate and complete throughout the process.

Risk Management and Contingency Planning
√ Configure Predictive Alerts
Set up the system to flag high-risk patients or potential referral delays using historical patterns and real-time data analysis.
√ Create Backup Procedures
Establish manual processes that can be activated if the system experiences downtime, ensuring referral processing continues without interruption.
√ Implement Communication Protocols
Set up automated updates to referring hospitals about referral status, including acceptance confirmations, clinical questions, or alternative recommendations.
Phase 5: Optimization and Continuous Improvement (Ongoing)
Performance Monitoring and Analytics
√ Track Key Performance Indicators
- Average referral processing time
- Referral acceptance rates by source and type
- Staff productivity improvements
- Patient satisfaction scores
- Revenue cycle improvements
√ Regular System Audits
Conduct monthly reviews of system performance, data accuracy, and user feedback to identify optimization opportunities.
√ Leverage Machine Learning Insights
Allow the platform’s AI algorithms to learn from your facility’s outcomes, continuously improving matching accuracy and recommendations over time.
Ongoing Training and Support
√ Schedule Regular Training Updates
Plan quarterly training sessions to cover new features, refresh user knowledge, and onboard new staff members.
√ Maintain Vendor Relationships
Establish regular communication with your AI referral management vendor for system updates, best practice sharing, and technical support.
√ Document Process Improvements
Keep detailed records of workflow changes and system optimizations to inform future technology decisions and staff training.
Implementation Success Factors
The most successful AI referral management implementations share several common characteristics. They prioritize robust training programs that ensure all staff members feel confident using the new system. They maintain strong relationships with referring hospitals through regular communication about system capabilities and referral outcomes.
Successful facilities also establish clear metrics for success and regularly review performance data to identify areas for continuous improvement. They understand that AI referral management is not a one-time implementation but an ongoing optimization process that evolves with their facility’s needs.
Ready to Transform Your Referral Process?
Implementing AI referral management can seem complex, but with this systematic approach, your skilled nursing facility can successfully transition to automated, efficient referral processing. The investment in time and resources during implementation pays dividends through faster bed fills, reduced administrative burden, and improved patient outcomes.
Ready to get started with AI referral management for your facility? Schedule a personalized demo to see how Smart Admissions can streamline your referral process and boost your facility’s efficiency