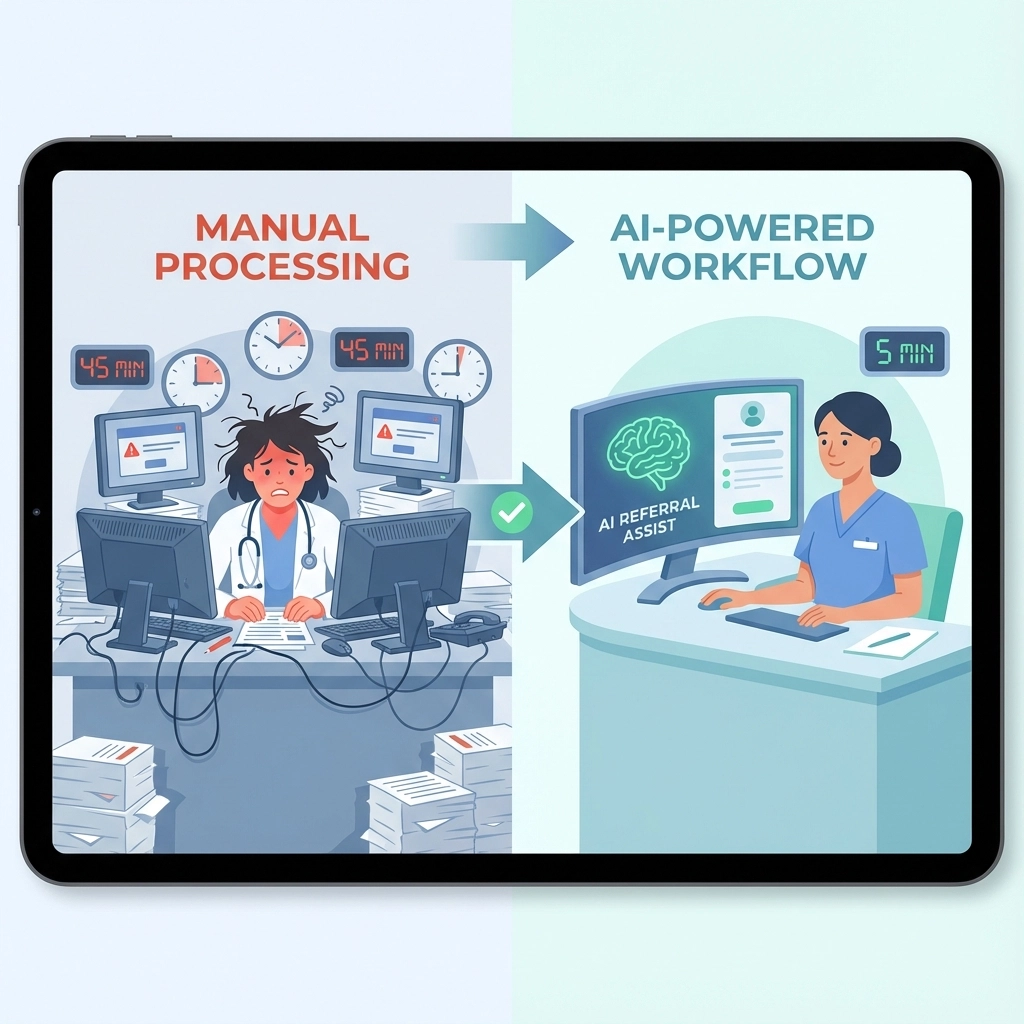
Picture this: Your admissions coordinator just received a referral at 2:47 PM. By traditional standards, they’d spend the next 45 minutes reviewing medical records, checking insurance eligibility, validating clinical requirements, and coordinating with nursing staff. But what if that same comprehensive review could happen in just 5 minutes?
This isn’t science fiction: it’s the reality that AI referral management is delivering to skilled nursing facilities across the country. The transformation is so dramatic that facilities implementing intelligent automation are processing 8x more referrals in the same timeframe, fundamentally changing how post-acute care admissions operate.
The 45-Minute Referral Review Reality
Before diving into the solution, let’s acknowledge the current reality most skilled nursing facilities face. A typical referral review involves multiple time-consuming steps:
Clinical Assessment (15-20 minutes): Manually reviewing medical histories, medication lists, diagnoses, and care requirements. Admissions staff must cross-reference clinical capabilities, check for contraindications, and ensure the facility can meet the patient’s needs.
Insurance Verification (10-15 minutes): Calling insurance providers, navigating automated phone systems, verifying coverage details, and confirming authorization requirements. This step alone can extend to hours if prior authorizations are needed.
Documentation Review (8-12 minutes): Examining discharge summaries, physician orders, recent lab results, and other medical documentation to build a complete picture of the patient’s condition and care requirements.
Internal Coordination (5-8 minutes): Consulting with nursing staff, dietary teams, therapy departments, and other specialists to confirm capacity and care capability.
This manual process isn’t just time-consuming: it’s error-prone. Studies show that manual referral processing leads to a 23% error rate in initial assessments, often requiring additional review cycles that further delay admissions decisions.
The AI Revolution in Referral Management
AI referral management systems are fundamentally restructuring this workflow through intelligent automation that processes information at machine speed while maintaining clinical accuracy. Here’s how the 5-minute transformation happens:
Instant Document Processing
Advanced natural language processing algorithms can scan and extract relevant information from medical records, discharge summaries, and clinical notes in seconds. The AI identifies key clinical indicators, medication interactions, care requirements, and potential red flags faster than human reviewers can read the first page.
Real-Time Insurance Validation
Instead of phone calls and hold times, AI systems connect directly to insurance databases and verification networks. Coverage details, authorization requirements, and benefit limitations are confirmed within 30-60 seconds, eliminating the longest bottleneck in traditional workflows.
Automated Clinical Matching
Machine learning algorithms compare patient needs against facility capabilities, staffing patterns, and current census data to determine fit probability. The system can instantly identify whether your facility has the clinical expertise, equipment, and capacity to provide optimal care.
Intelligent Risk Assessment
AI analyzes patterns across thousands of similar cases to predict potential complications, readmission risks, and care complexity. This gives admissions teams crucial insights that would take experienced clinicians significant time to develop manually.
The Efficiency Transformation in Action
The transformation from 45 minutes to 5 minutes isn’t just about speed: it’s about efficiency transformation that creates competitive advantages across multiple dimensions:
Increased Response Velocity
Facilities using AI referral management respond to referral opportunities 8x faster than competitors. In an environment where hospitals and case managers often award referrals to the first facility that responds comprehensively, this speed advantage translates directly to increased admissions.

Enhanced Decision Quality
Counter-intuitively, faster processing often means better decisions. AI systems can analyze more variables simultaneously than human reviewers, identifying subtle patterns and potential issues that might be overlooked in manual reviews. This leads to better patient-facility matches and improved outcomes.
Staff Resource Optimization
With referral reviews automated, admissions coordinators can focus on relationship building, complex case coordination, and patient/family communication. This shift from administrative tasks to high-value activities improves both job satisfaction and facility performance.
Real-World Applications and Time Savings
Successful implementations demonstrate the time savings potential across different facility types:
150-bed skilled nursing facility: Reduced average referral processing from 42 minutes to 4.5 minutes, enabling the admissions team to review 200% more referrals per day while maintaining clinical quality standards.
Multi-facility post-acute care network: Standardized review processes across locations, reducing training time for new admissions staff by 70% while ensuring consistent clinical decision-making protocols.
Rehabilitation-focused SNF: Automated therapy screening and capacity matching reduced referral-to-admission timeframes by 60%, improving relationships with referring hospitals and increasing competitive positioning.
Key Features Driving the Transformation
Intelligent Document Analysis
Modern AI systems use optical character recognition combined with medical language processing to extract relevant information from handwritten notes, printed reports, and electronic health records. The technology understands medical terminology, dosage calculations, and clinical relationships that would require specialized training for human reviewers.
Predictive Analytics Integration
Beyond processing current information, AI referral management systems analyze historical patterns to predict care trajectories, length of stay, and resource requirements. This forward-looking capability helps facilities make more informed admission decisions and better resource planning.

Automated Workflow Orchestration
AI doesn’t just process individual referrals: it manages entire workflow sequences. From initial screening through insurance verification to care team notification, the system coordinates multiple parallel processes that would traditionally require manual handoffs and follow-up.
Real-Time Capacity Matching
Dynamic integration with facility management systems ensures that bed availability, nursing ratios, therapy schedules, and specialized care capabilities are considered in real-time. This eliminates the common problem of accepting referrals that stretch facility resources beyond optimal levels.
Implementation Considerations for Maximum Impact
Change Management Strategy
The transition to AI-powered referral management requires thoughtful change management. Staff training should focus on leveraging AI insights rather than replacing clinical judgment. The most successful implementations position AI as a powerful tool that enhances human decision-making rather than a replacement for clinical expertise.
Integration Requirements
Effective AI referral management requires integration with existing systems including electronic health records, facility management software, and insurance verification platforms. The complexity of these integrations varies, but modern solutions offer API-based connections that minimize disruption to current workflows.
Quality Assurance Protocols
While AI dramatically improves speed and consistency, human oversight remains crucial for complex cases and exceptional circumstances. Establishing clear protocols for when to escalate to human review ensures that automation enhances rather than compromises clinical decision-making.
The Competitive Advantage of Speed
In today’s post-acute care market, referral response speed has become a critical differentiator. Hospitals and case managers increasingly award referrals to facilities that can respond quickly with comprehensive information. The transformation from 45 minutes to 5 minutes creates several competitive advantages:
First-mover advantage: Being the first facility to respond to time-sensitive referrals significantly increases admission probability.
Relationship strengthening: Consistent rapid responses build trust with referring partners and establish facilities as preferred providers.
Operational efficiency: Processing more referrals in less time improves facility utilization and financial performance.

The facilities that embrace AI referral management today are positioning themselves to capture a disproportionate share of referrals tomorrow. As this technology becomes standard, facilities still relying on manual processes will find themselves increasingly disadvantaged in competitive referral situations.
Looking Forward: The Future of Intelligent Admissions
The evolution from 45-minute to 5-minute referral reviews represents just the beginning of AI’s impact on post-acute care admissions. Future developments will likely include predictive referral matching, automated outcome tracking, and intelligent capacity optimization that further streamlines the entire admissions ecosystem.
Facilities considering this transition should evaluate their current referral volume, processing capabilities, and competitive positioning. The question isn’t whether AI will transform referral management: it’s whether your facility will be an early adopter capturing competitive advantages or playing catch-up in an increasingly automated market.
Ready to transform your referral processing from 45 minutes to 5? Book a demonstration to see how AI referral management can revolutionize your admissions workflow and give your facility the competitive edge it needs to thrive in today’s post-acute care market.
Tags: ai referral management, admissions automation healthcare, streamline referral process, automated patient intake, skilled nursing facility admissions, fill nursing home beds faster, post-acute care software