When it comes to patient intake in skilled nursing facilities, administrators face a critical decision that impacts everything from staff productivity to patient outcomes. Should you stick with traditional manual processes, or make the leap to automated patient intake systems?
The data tells a compelling story. Facilities using automated patient intake systems consistently outperform their manual counterparts across every measurable metric that matters to your bottom line and patient care quality.
The Current State of Manual Patient Intake
Most skilled nursing facilities still rely heavily on manual processes for patient intake. This typically involves staff members manually reviewing referral documents, extracting key information by hand, making phone calls for verification, and entering data into multiple systems.

While this approach has been the standard for decades, it creates significant operational challenges:
Time-Intensive Processing: Manual intake processes can take up to 12 hours from referral receipt to admission decision. Staff spend 30 minutes or more just preparing and auditing paperwork for each admission.
Sequential Bottlenecks: Manual workflows force tasks to happen one after another. You can’t verify insurance until someone manually extracts the policy information. You can’t begin care planning until someone transcribes the clinical notes. Each step waits for the previous one to complete.
Error-Prone Data Entry: When staff manually enter information from handwritten notes or poorly scanned documents, errors are inevitable. These mistakes cascade through the entire care process, affecting everything from medication management to therapy planning.
How Automated Patient Intake Transforms Operations
Automated patient intake systems use artificial intelligence to extract, verify, and organize patient information without human intervention. Instead of staff manually reading through documents, AI systems can process multiple referrals simultaneously, extracting relevant data points and flagging important clinical information.
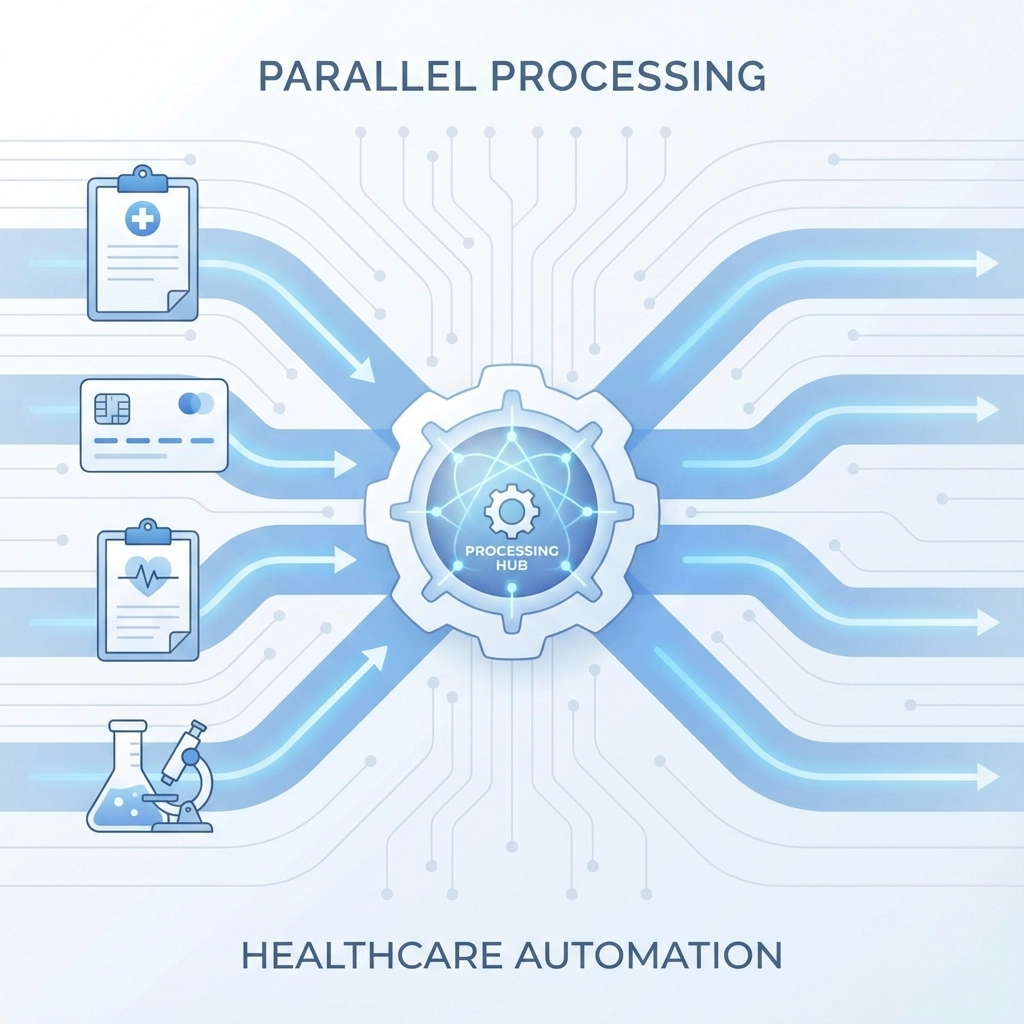
Parallel Processing Power: Unlike manual systems that handle one task at a time, automation can simultaneously extract patient demographics, verify insurance coverage, process physician orders, and begin care plan development. This parallel processing eliminates the sequential bottlenecks that slow down manual systems.
Instant Data Extraction: AI systems can review a 50-page referral packet and extract all relevant clinical, demographic, and insurance information in under 5 minutes. What once required staff to manually review and transcribe now happens automatically.
Real-Time Verification: Automated systems can instantly verify insurance benefits, check bed availability, and cross-reference clinical requirements against facility capabilities: all without human intervention.
Speed: The Numbers Don’t Lie
The speed difference between manual and automated intake is dramatic:
- Overall admission timeline: Automated systems reduce the referral-to-admission process from approximately 12 hours to under 2 hours
- Document preparation: Paperwork prep and audit time drops from 30 minutes to 5 minutes per case
- Bottleneck reduction: Facilities report 75% fewer processing bottlenecks with automated systems
- High-acuity cases: Complex referrals are reviewed and approved 90% faster with automation
This speed advantage directly translates to competitive advantage. In today’s market, the first facility to respond to a referral often wins the admission. When your competitors are still manually processing referrals hours later, your automated system has already made the admission decision and contacted the referring hospital.
Accuracy and Quality Improvements
Manual data entry creates systematic accuracy problems that affect patient care:
Human Error Rates: Staff transcribing information from paper documents or poor-quality faxes inevitably make mistakes. These errors compound as incorrect information moves through your systems.
Incomplete Information: Manual processes often result in missing data points. When clinicians don’t have complete information, they’re forced to make assumptions that can compromise care quality.
Automated systems achieve approximately 100% accuracy on clinical and demographic data extraction. They don’t get tired, distracted, or overwhelmed during busy periods. Every data point extracted from source documents is captured consistently and accurately.
Financial Impact: What Manual Processes Really Cost
The financial implications of intake method choice are substantial:
Delayed Admission Costs: Every 24-hour delay in processing an admission costs approximately $450 per bed in lost revenue. Manual processes that take 12+ hours to complete create expensive delays.
Empty Bed Days: Facilities using automated intake systems reduce empty bed days by 15-20% within four months of implementation. This improvement comes from faster processing and higher referral conversion rates.
Administrative Labor Costs: Manual intake consumes significant staff time. Automated systems save approximately 60% of admission team bandwidth, allowing existing staff to handle more volume or focus on higher-value activities.
Process Efficiency: Facilities report average monthly savings of $700 by eliminating paper-based manual processes and the associated printing, storage, and handling costs.
Staff Impact and Job Satisfaction
Manual intake processes contribute significantly to staff burnout in skilled nursing facilities. Admission coordinators and nurses spend hours each day on repetitive data entry tasks instead of focusing on patient care activities that drew them to healthcare.
Reduced Burnout: Automation eliminates the most tedious aspects of intake processing. Staff report higher job satisfaction when freed from repetitive manual tasks.
Better Resource Allocation: With 60% more bandwidth available, admission teams can provide more personalized attention to complex cases, spend more time on relationship building with referral sources, and focus on care coordination activities.
Improved Retention: Facilities often see improved retention rates among admission staff after implementing automation, as job roles become more strategic and less administrative.
Compliance and Risk Management
Manual processes create compliance risks that automated systems eliminate:
Documentation Completeness: Manual workflows often result in incomplete documentation. Staff may miss required signatures, skip data fields, or fail to complete audit trails properly.
Regulatory Compliance: Automated systems provide real-time visibility into documentation compliance. Administrators can instantly verify completion rates, track electronic signatures, and identify missing information before regulatory audits.
Clinical Risk Reduction: When care teams receive incomplete or inaccurate information from manual intake processes, they must make clinical decisions based on assumptions. Automated systems ensure clinical staff always have complete, accurate information at the point of care.

Patient Outcomes and Satisfaction
The intake process directly impacts patient care quality and satisfaction:
Care Transition Issues: Manual intake delays contribute to 30% of patient satisfaction complaints and 25% of preventable readmissions when care transitions are compromised by administrative inefficiencies.
Faster Care Planning: With complete, accurate information available immediately upon admission, clinical teams can begin appropriate interventions faster. This leads to better patient outcomes and shorter lengths of stay.
Communication Improvements: Automated systems eliminate the communication breakdowns common in manual processes, ensuring all team members have access to the same accurate information simultaneously.
Making the Decision: Is Automation Right for Your Facility?
Given the overwhelming evidence favoring automated patient intake, the question isn’t whether automation is better: it’s whether your facility can afford to continue with manual processes.
Consider these decision factors:
Volume Considerations: If your facility processes more than 10-15 admissions per month, the time savings from automation will generate positive ROI within months.
Competitive Environment: In markets where multiple SNFs compete for the same referrals, response speed often determines who gets the admission.
Staff Resources: If your admission team is overwhelmed, experiencing high turnover, or struggling to keep up with volume, automation can provide immediate relief.
Quality Goals: Facilities focused on improving patient outcomes and satisfaction scores will see measurable improvements from automated intake processes.
The Path Forward
The evidence is clear: automated patient intake systems deliver superior performance across every metric that matters to skilled nursing facilities. From speed and accuracy to cost savings and staff satisfaction, automation provides measurable advantages over manual processes.
The question facing facility administrators isn’t whether to automate, but how quickly they can implement these systems before competitors gain the advantage.
Ready to see how automated patient intake can transform your facility’s operations? Schedule a personalized demo to discover how much time and money your facility could save with intelligent automation.
Tags: automated patient intake, skilled nursing facility admissions, admissions automation healthcare, ai referral management, streamline referral process, post-acute care software, fill nursing home beds faster