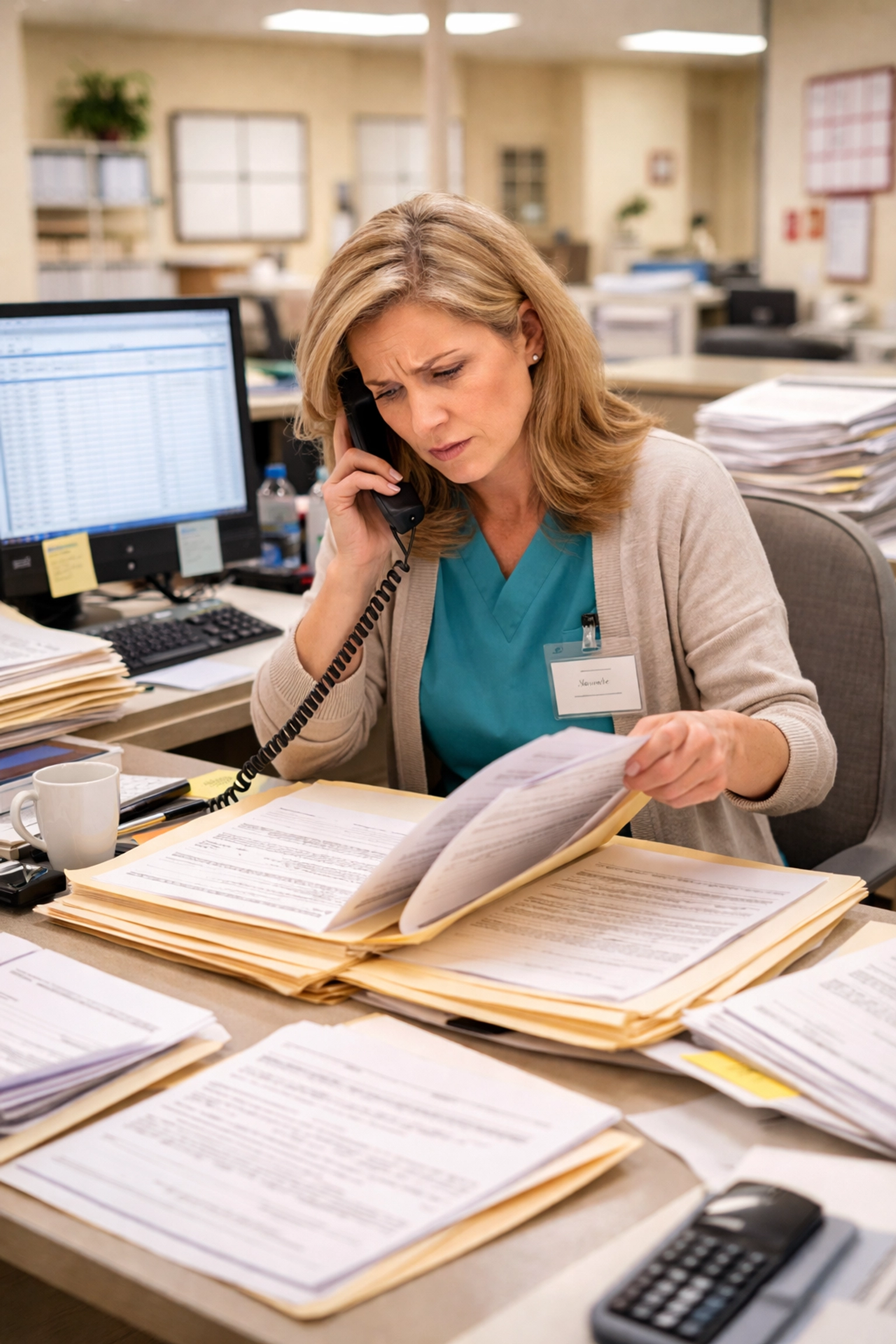
If you’re an admissions coordinator at a skilled nursing facility, you already know the headache of DD214 verification. The good news? You can streamline your referral process and reclaim hours of your week without sacrificing accuracy or compliance.
Right now, DD214 verification consumes 15-20 minutes per referral at most facilities. When you’re processing 50+ veteran referrals weekly, that adds up to 12.5-16.7 hours of pure admin time. That’s time you could spend actually filling beds and caring for residents.
This guide breaks down exactly how to cut that admin burden by 50-70% while improving your acceptance rates.
Why DD214 Verification Creates Such a Bottleneck
Let’s be honest about what’s happening at most SNFs today. Your team receives a veteran referral, and then the scramble begins. Someone has to locate the DD214, verify military service dates, confirm discharge status, and cross-reference everything with VA payment eligibility.
Each step involves manual data entry, phone calls, and waiting. Meanwhile, that bed sits empty and competing facilities are responding faster.
The real cost isn’t just time. It’s the referrals you lose because your response took too long. Hospital discharge planners work with whoever responds first. If your verification process takes hours while a competitor responds in minutes, you’re losing revenue every single day.
3 Ways to Streamline Your Referral Process for DD214 Verification
Here’s where things get actionable. These strategies come directly from facilities that have cut their admin time dramatically.
1. Eliminate Unnecessary Documentation Barriers
Start by questioning which documents you actually need before admission. Many facilities require paperwork that duplicates information already available through VA systems.
According to the VA’s Grant & Per Diem program guidelines, you can often replace DD214 requirements entirely with VA data verification. Consider these swaps:
- Replace DD214 with VA medical center data when possible
- Accept VA ID cards instead of requiring state identification
- Use VA verification letters instead of Social Security cards
Work with your compliance team to identify which intake steps can be consolidated or eliminated. You might be surprised how many redundant requirements have accumulated over time.
2. Leverage Existing VA Verification Systems
Stop relying solely on manual verification when automated tools exist. The VA offers several systems that can speed up your eligibility decisions.
SQUARES provides immediate eligibility decisions when VA medical center staff aren’t available for real-time verification. This alone can shave significant time off each referral.
Additionally, the VA HOMES Reporting Policy allows direct admissions without requiring VA staff to meet with veterans prior to program entry. If you’re not using this pathway, you’re creating unnecessary delays.

Train your entire admissions team on these tools. When everyone knows how to access eligibility information quickly, you eliminate single points of failure in your process.
3. Optimize Your Intake Schedule
If your facility only conducts intakes a couple times per week, you’re building delays into your system. Every day a veteran waits is a day that bed generates zero revenue.
Consider implementing daily on-the-spot intakes. Yes, this requires staffing adjustments. But facilities that offer same-day access consistently fill beds faster than those with rigid intake schedules.
Real-time bed availability updates also matter. When your team knows exactly which beds are open, they can accept appropriate referrals immediately instead of playing phone tag with nursing staff.
The Case for DD214 Automation Technology
Manual process improvements only take you so far. To truly streamline your referral process and achieve that 50-70% time savings, automation becomes essential.
Modern DD214 automation technology can reduce verification time from 15-20 minutes to literal seconds. Here’s how it works:
When a referral enters your system, the software simultaneously validates military eligibility and confirms VA payment eligibility. No manual lookups. No phone calls. No waiting for callbacks from the VA.
This isn’t science fiction. Facilities using automated verification systems report dramatic improvements in both speed and accuracy.

The accuracy piece matters more than you might think. Manual verification introduces human error at every step. Automated systems pull directly from authoritative sources, reducing claim denials and payment delays down the road.
What 50-70% Time Savings Actually Looks Like
Let’s put real numbers to these improvements. Say your facility processes 50 veteran referrals per week, and each one currently takes 18 minutes to verify.
Current state: 50 referrals × 18 minutes = 900 minutes (15 hours) weekly
After optimization: 50 referrals × 5 minutes = 250 minutes (4.2 hours) weekly
That’s 10.8 hours returned to your admissions team every single week. Over a year, you’re looking at 560+ hours: equivalent to nearly three months of full-time work.
What could your team accomplish with that time? More facility tours. Faster responses to hospital discharge planners. Better relationships with referral sources. All of these translate directly to higher occupancy rates.
Avoiding Common DD214 Verification Mistakes
Even with optimized processes, certain mistakes can undermine your efficiency gains. We’ve documented the 7 DD214 verification mistakes that cost facilities thousands, and they’re worth reviewing.
The most expensive error? Accepting referrals without confirming VA payment eligibility upfront. A verified DD214 doesn’t automatically mean the VA will pay for SNF care. You need both pieces confirmed before admission.
Another common pitfall is failing to establish clear handoff procedures between shifts. When verification tasks fall through the cracks during shift changes, referrals get delayed and sometimes lost entirely.
Getting Started: Your First Week Action Plan
You don’t need to overhaul everything at once. Start with these steps:
Day 1-2: Audit your current DD214 verification process. Time each step and identify where delays occur.
Day 3-4: Review your documentation requirements with compliance. Eliminate anything redundant.
Day 5: Train your team on VA verification tools like SQUARES if you’re not already using them.
Week 2 onward: Evaluate automation solutions that can handle the heavy lifting. Smart Admissions offers instant eligibility verification that integrates with your existing workflow.
The Bottom Line for Admissions Coordinators
Your time is too valuable to spend on repetitive verification tasks that technology can handle in seconds. The facilities winning the most referrals right now are the ones responding fastest: and you can’t respond fast when you’re buried in manual DD214 lookups.
The path forward is clear. Eliminate unnecessary barriers, leverage existing VA systems, optimize your intake schedule, and seriously consider automation for high-volume verification tasks.
Ready to see how much time your facility could save? Start a free trial and experience what it feels like to streamline your referral process from day one.
Focus Keyword: streamline referral process
Categories: AI Referral Management, Skilled Nursing Facility Admissions, Insurance Verification Healthcare
Tags: automated patient intake, fill nursing home beds faster, streamline referral process, admissions automation healthcare, DD214 verification, veteran SNF admissions, real-time referral response